





Better Gut
BestsellerTargeted Biotic Supplement
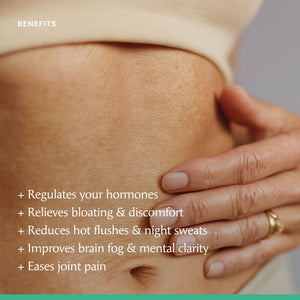
Better Gut is a biotic supplement formulated to support female gut health and the gut–hormone connection.
During perim...Read More
Better Gut is a biotic supplement formulated to support female gut health and the gut–hormone connection.
During perimenopause, natural changes in oestrogen can affect the balance of bacteria in the gut microbiome.
Developed by doctors, Better Gut combines six carefully selected bacterial strains, delivering 50 billion live CFUs per capsule to help maintain balance and overall wellbeing.
For best results, take consistently for at least 3-months.
Read Less- Tiredness & fatigue
- Optimal gut function
- Healthy sleep
- Overall vaginal health
- 3- months supply delivered every 3 months
- Free UK shipping
- Pause, skip, or cancel anytime
- Earn 3% store credit
- 1-month supply delivered monthly
- Free UK shipping
- Pause, skip, or cancel anytime
- Earn 3% store credit
Store pickup unavailable

5 / 5
5 / 5
"I love Better Gut. It is the one product I prioritise. It has transformed my digestive health and sorted out my perimenopausal bloating. I highly recommend it to you."
The gut–hormone connection explained
The gut–hormone connection explained
Most of us know how important gut health is for digestion, immunity, and overall wellbeing. What’s less well known is how closely your gut and hormones communicate, and how strongly that connection can shape how you feel during perimenopause and beyond.
During this time, as oestrogen levels rise and fall, they can disrupt the delicate balance of gut bacteria known as the estrobolome. These bacteria help your body process and regulate oestrogen, supporting everything from mood and sleep to energy and bone health.
When this balance becomes unsettled, symptoms like bloating, brain fog, and low mood can become more noticeable. Supporting your gut with the right beneficial bacteria can help you feel more comfortable, steady, and resilient through these hormonal changes.
Better Gut was created by women’s-health experts to nurture this vital gut–hormone connection. Each daily capsule delivers 50 billion CFU from six clinically studied probiotic strains, simple, science-backed support, whether you’re taking HRT or not.
Clinically studied, targeted strains for daily support
Clinically studied, targeted strains for daily support
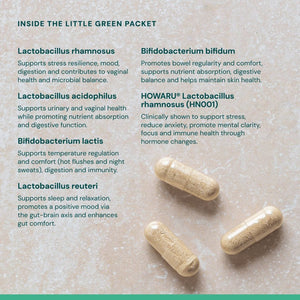
Every capsule of Better Gut contains six carefully selected bacterial strains, chosen for their proven ability to support gut health and overall wellbeing during perimenopause and beyond.
Each one plays a role in helping your body stay balanced and resilient through hormonal change.
The 6 Key Strains
Lactobacillus rhamnosus – Supports stress resilience and helps ease bloating and inflammation.
Lactobacillus acidophilus – Helps maintain vaginal health and supports urinary comfort.
Bifidobacterium lactis – Linked to reduced hot flushes and night sweats.
Lactobacillus reuteri – Supports mood balance and sleep quality.
Bifidobacterium bifidum – Aids regular digestion and relieves constipation.
HOWARU® Lactobacillus rhamnosus – Helps support emotional wellbeing and stress management.
Each capsule delivers 50 billion CFU, providing daily, targeted support for your gut and hormonal health.
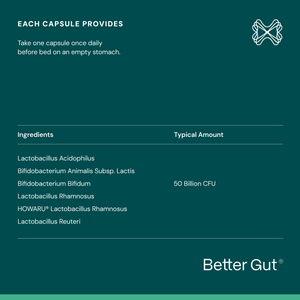
Ingredients
Micro-organisms (Lactobacillus acidophilus, Lactobacillus reuteri, Lactobacillus rhamnosus, Bifidobacterium animalis subsp. lactis, HOWARU® Lactobacillus rhamnosus, Bifidobacterium bifidum), Vegetable Capsule Shell (Hydroxy Propyl Methyl Cellulose), Bulking Agent (Microcrystalline Cellulose), Anti-Caking Agents (Rice Bran, Ascorbyl Palmitate, Magnesium).
Allergy Advice
- No allergenic ingredients
- No artificial colours, flavours or preservatives
- Gluten-free
- Dairy-free
- Suitable for vegetarians and vegans
Important Information
Do not use if inner seal is broken. Keep out of the sight and reach of children.
Food supplements should not be used as a substitute for a varied diet and healthy lifestyle.
Consult a doctor or healthcare professional before use if you are pregnant, breastfeeding, taking medication or under medical supervision.
Store in the original packaging, in a cool, dry place below 25°C.
Simple to take, easy to fit into your routine
Simple to take, easy to fit into your routine
Taking Better Gut is simple and designed to fit easily into your daily routine.
- Take one capsule every day with a glass of water.
- You can take it first thing in the morning or before bed, whichever suits you best.
- No need to refrigerate. Store it in a cool, dry place away from direct sunlight.
Before assessing results, we recommend taking Better Gut for at least 3-months to allow your microbiome time to rebalance and respond.
It is formulated for everyday use to support your body’s changing needs through perimenopause and beyond.
Can be taken alongside HRT.
Flexible subscriptions for consistent, reliable support
Flexible subscriptions for consistent, reliable support
Better Gut works best when taken daily, helping to build lasting balance in your gut microbiome. Our flexible subscription plans makes it easy to stay consistent and never miss a day, at our best price, plus you get...
- Free delivery on every order
- Fast shipping within 2 to 3 days (orders placed before 1pm ship the same day)
- Pause, skip, or cancel anytime for complete flexibility
- Choose from 4-week or 12-week subscription plans
- Get 3% store credit with every order
Subscribing ensures your next supply of Better Gut arrives right when you need it, so you can continue feeling your best without interruption.
Think of it as your daily foundation in your menopause toolkit, helping you stay supported and steady through every stage.
We recommend taking Better Gut for at least 3-months before reviewing your results, giving your body time to adjust and experience the full benefits.


“Real relief in menopause starts in your gut.”
Press play to hear Dr Shahzadi Harper explain the science behind Better Gut and how it supports women through perimenopause and beyond.
-
"A probiotic made with clinically proven ingredients can make a real difference"
-

"Gut health could be the non-medical solution to menopause symptoms"
-

"The right blend of probiotics can be a game-changer for your menopause"
-
"Better Gut is the best probiotic for women in perimenopause and beyond"














Mandy
Customer
"After about two weeks of taking Better Gut I really started to notice the difference, I was sleeping much better, my mood was much calmer and my anxiety levels were much lower."
Kate
Customer
"My night sweats have now completely gone, I have nothing but postive things to say about Better Gut."
Jo
Customer
"Since entering perimenopause, my bloating got even worse, even painful. I discovered Better Gut and I've never looked back, a year on and I wouldn't be without it."
Kate
Customer
"Better Gut has been a game-changer for me, my bloating, gassiness after eating is so much better and I know I'm doing my gut bacteria a whole world of good."
Dr Shari. Daniels
Customer
I take Better Gut daily, honestly, I wouldn't be without them, it's my a huge difference to how I feel."
Jane
Customer
Laura
Customer
"Better Gut has made a huge difference to my everyday life, i'm so grateful to have found it, thank you to the team for creating such a great product, that really makes a difference."








Anna Poyser
Customer and Physiotherapist
"Gut health in perimenopause is so important, Better Gut has made a huge difference to my symptoms."
Debbie Wosskow OBE
Founder of The Better Menopause
Debbie shares her story from burnout to establishing The Better Menopause and the vision driving our range of supplements.
Jo Lyall
Head of Nutrition at The Better Menopause
"Can Better Gut be taken alongside HRT?"
Dr.Shahazdi Harper
Women's Health Specialist and Resident Doctor at The Better Menopause.
"When it comes to managing your menopause symptoms, Better Gut can make a huge difference."
Science-backed strains for targeted support
Better Gut isn’t just another general probiotic. Our experts have selected six scientifically studied strains best suited to support your gut microbiome and hormonal balance during perimenopause and beyond.
Lactobacillus Rhamnosus
Lactobacillus rhamnosus GG is a lactic acid bacteria (LAB) known for improving digestive issues, IBS & protecting the lining of your gut.
Benefits:
- Relieves hot flushes & night sweats
- Lowers anxiety & depression risk
- Supports gut barrier & stress resilience

Bifidobacterium lactis
Bifidobacterium lactis helps to boost immune function, and helps ease bloating and constipation with the benefits shown in several clinical studies.
Benefits:
- Supports healthy digestion and regular bowel movements.
- Strengthens immune response and gut barrier function.
- Reduces bloating and improves overall gut comfort.

HOWARU® Lactobacillus rhamnosus
HOWARU® Lactobacillus is a clinically studied probiotic that supports vaginal and urinary tract health, improves digestive comfort, and helps strengthen immune and emotional resilience in women during perimenopause and beyond.
Benefits:
- Supports vaginal and urinary tract health by maintaining healthy microflora.
- Promotes digestive comfort and regularity.
- Enhances immune balance and emotional well-being during perimenopause and beyond.

Lactobacillus acidophilus
Lactobacillus acidophilus supports digestive balance, enhances immune defense, and helps maintain healthy vaginal flora.
Benefits:
- Supports vaginal and urinary tract health
- Enhances digestion and nutrient absorption, easing bloating and gut discomfort.
- Strengthens immune function and may reduce inflammation linked to ageing

Lactobacillus reuteri
Lactobacillus reuteri supports vaginal balance, reduces inflammation, and can help to maintain bone density during perimenopause and beyond.
Benefits :
- Reduces inflammation
- Relieves vaginal dryness and inflammation
- Lowers osteoporosis risk

Bifidobacterum Bifidum
Bifidobacterium bifidum supports digestive balance, strengthens immune health, and helps maintain skin and gut well-being.
Benefits:
- Supports healthy digestion and relieves bloating or bowel irregularity.
- Strengthens immune defenses and reduces inflammation.
- Promotes skin health and overall gut–skin balance.

-

Targeted, science backed strains for (peri) menopause
-

High-strength, 50 billion CFUs in every capsule
-

Blister-sealed capsules keep the live bacteria fresh
-

Simple, once-daily capsule – no taste, no liquid
-

Formulated by women for women in perimenopause
-

Clinically informed formulation for the female microbiome
-

Targeted, science backed strains for (peri) menopause
-

High-strength, 50 billion CFUs in every capsule
-

Blister-sealed capsules keep the live bacteria fresh
-

Simple, once-daily capsule – no taste, no liquid
-

Formulated by women for women in perimenopause
-

Clinically informed formulation for the female microbiome
What to expect on your Better Gut journey

What to expect on your Better Gut journey
Weeks 1–4: Many women start to feel lighter and less bloated. You may notice more comfortable digestion and a greater sense of calm as your body adjusts to consistent daily support.
Weeks 4–8: With regular use, you might experience steadier energy, improved mood, and fewer digestive fluctuations. Many women also report a lift in brain fog at this point.
Weeks 8–12: By now, your gut microbiome is better supported, helping you feel more balanced and comfortable day to day. Bloating, fatigue, and mood changes may continue to ease as consistency pays off.
Beyond 12 Weeks: Better Gut becomes part of your daily rhythm, maintaining comfort, supporting natural hormone balance, and helping you feel more like yourself again. With continued use, many women also notice benefits for their skin, hair, and overall vitality.
Real results from women feeling the difference
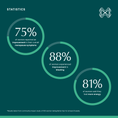
After just two months of taking one daily capsule of Better Gut, participants in our impact study experienced relief from a range of common menopausal symptoms.
experienced a significant improvement in bloating
saw an improvement in their overall menopause symptoms
reported a noticeable improvement in overall energy levels
Still have questions? we’re here for you
We know finding the right support can feel confusing. You’ll find answers to our most commonly asked questions below. If you still need help, just tap 'contact us' below.
Can I take Better Gut throughout perimenopause and then post menopause?
Can I take Better Gut throughout perimenopause and then post menopause?
Yes, maintaining gut health throughout perimenopause, menopause, and beyond is both scientifically supported and highly beneficial.
Oestrogen is a systemic hormone that influences almost every cell in the body. It plays a key role in maintaining bone density, cardiovascular function, cognitive health, skin integrity, and muscle strength.
It also affects immune responses, inflammation, and has a direct impact on the composition and function of the gut microbiome.
As oestrogen levels begin to fluctuate and later decline after menopause, these systems can become more vulnerable.
The gut microbiome, in particular, can lose some of its diversity, which may contribute to common symptoms such as bloating, fatigue, and changes in mood or digestion.
Supporting your gut with Better Gut helps maintain microbial balance, reduce inflammation, and promote overall physiological resilience. It may also support more effective nutrient absorption, which is vital for bone and immune health, especially after menopause when oestrogen levels are lower.
Better Gut is designed to be taken safely and effectively daily throughout perimenopause, menopause, and well beyond as part of your daily wellbeing routine.
Is Better Gut safe to take with HRT?
Is Better Gut safe to take with HRT?
Yes, Better Gut can be safely taken alongside Hormone Replacement Therapy (HRT).
In fact, they can work well together. While HRT supports the replenishment of oestrogen and progesterone levels, Better Gut focuses on the gut and hormone connection, helping to balance the microbiome, aid digestion, and support your body’s natural ability to metabolise hormones effectively.
By supporting gut health, Better Gut may also help your body make the most of the nutrients that contribute to overall wellbeing, which can be especially important while taking HRT.
As with any supplement, if you have specific medical conditions or are taking prescribed medication, it’s always best to check with your GP or healthcare professional first.
Together, HRT and Better Gut can form part of a holistic approach to menopause care, combining medical support with daily, science-backed nutrition for comfort and balance.
How do I take Better Gut?
How do I take Better Gut?
Take one capsule daily with a glass of water. You can take it either first thing in the morning or in the evening before bed, whatever fits best into your routine.
There’s no need to refrigerate Better Gut, as each capsule is individually blister sealed to ensure the live bacteria stay protected and effective.
Simply store it in a cool, dry place away from direct sunlight.
Consistency is key. Better Gut is designed to be taken every day to support the natural rhythm of your gut microbiome and deliver lasting results.
We recommend taking it for at least 12 weeks to allow your gut to fully adjust and experience the best benefits.
Better Gut can be taken safely alongside HRT and other supplements.
Think of it as your daily foundation for wellbeing through perimenopause, menopause, and beyond.
Is Better Gut free from common allergens and additives?
Is Better Gut free from common allergens and additives?
Yes. Better Gut is free from artificial colours, flavours, and preservatives.
It also contains no allergens, GMOs, gluten, dairy, or animal ingredients.
Each capsule is vegetarian and made from plant-based hydroxypropyl methyl cellulose, with no gelatin, fillers, or binders.
What is the significance of 50-billion CFUs?
What is the significance of 50-billion CFUs?
CFU stands for colony-forming units, which is how the number of live, active bacteria in a probiotic is measured.
Each capsule of Better Gut contains 50 billion CFU, meaning 50 billion live cultures are delivered to your gut every day. This amount has been carefully selected by our experts to provide a powerful and effective dose that supports meaningful results without overwhelming your natural microbiome.
It’s designed to strike the right balance between strength and gentleness, delivering daily support that works in harmony with your body for long-term gut and hormone health.
Can I take Better Gut post cancer treatment?
Can I take Better Gut post cancer treatment?
Better Gut has no known contraindications for use following breast or ovarian cancer treatment, and it is considered safe to take alongside aromatase inhibitors.
However, it’s always important to speak with your doctor or specialist before adding any supplement to your routine after cancer treatment, so they can make sure it’s right for your individual health needs.
Better Gut is not recommended for individuals with severely compromised immune systems, those at risk of opportunistic infections, or those with significantly damaged gastrointestinal tracts.
If you’re unsure, your healthcare provider can help you decide the best time to introduce Better Gut as part of your recovery and long-term wellbeing plan.
Build on your Better Gut foundation your way
- DMDonna M.Verified BuyerI recommend this productRated 5 out of 5 stars1 week agoFeeling better already!
Have been taking these for 3 weeks now and already notice a difference with my gut. When I go to the toilet I am passing a proper stool! I notice a difference with my bloating too so feeling so much better. I have now got these on a subscription as I want to feel more good benefits. These truly work! Thank you x
Was this helpful? - LJLucy J.Verified BuyerI recommend this productRated 5 out of 5 stars1 week agoFeel amazing
I stopped my HRT due to not feeling much better & came across this product. I feel really good and back to my old self, no anxiety , moods stabilised & no irritation. I do keep thinking this is too good to be true but well done Better Gut am sold.
Was this helpful? - VHVanda H.Verified BuyerI recommend this productRated 5 out of 5 stars3 weeks agoThis has really worked for me!
I’ll admit I was initially skeptical about brands that promise to be a “one-stop shop” for menopause support — there are so many ads out there for supplements, shakes, and miracle fixes. However, after doing some research into the link between the gut microbiome and hormone balance, I decided to give Better Gut a try. The science behind it, Dr Harper — and the numerous great reviews convinced me it was worth a go.
After six weeks of taking it regularly, I can genuinely say I’ve noticed a real difference in my symptoms. I had been struggling with very itchy ears, scalp psoriasis, and poor sleep, and all three have improved noticeably. My scalp is now almost completely clear, the constant itching has stopped, and I’m sleeping much better. My digestion has also greatly improved. I used to have IBS flare ups from time to time and some digestive issues around my period and these seem to have lessened also!
I’m so glad I decided to start taking these probiotics and plan to continue. I’ve already recommended them to several friends because they’ve made such a positive difference to my day-to-day life.
Thank you, Better Menopause! ☺️
Was this helpful?The Better Menopause2 weeks agoThat's so great to hear, Vanda, thank you so much for taking the time to write such a detailed review.
- CSCarol S.Verified BuyerI recommend this productRated 5 out of 5 stars1 month agoLess IBS!
I have been taking these for nearly 2 months on recommendation from Eva Speakman. I have found I have less bloating, andthe pain that goes with that. Also , less IBS symptoms, especially the urgency.
Was this helpful? - CMCalogera M.Verified BuyerI recommend this productRated 5 out of 5 stars1 month agoGreat gut health benefits
Brilliant
Was this helpful?
Discover more on The Better Menopause edit
Menopause lower back pain: what causes it and what can help?
We explore the links between perimenopause, menopause and lower back pain, and look at some of the approaches that could provide relief.
Read moreThe Estrobolome: Why your gut–hormone connection matters in perimenopause
Discover how your gut microbiome, known as the estrobolome, affects oestrogen balance and perimenopause symptoms — and how to support it naturally.
Read moreWhy frozen shoulder is so common during menopause, and what helps
Learn why frozen shoulder affects midlife women, how menopause impacts joint health, and what you can do to reduce inflammation and recover naturally.
Read moreHow to stay cool during perimenopause: Natural relief for hot fushes, burning feet & hormonal heat
Perimenopause can feel like someone turned up the thermostat on your life. Whether you’re suddenly sweating through your clothes in a meeting or waking in the middle of the night with burning feet and a flushed face, you’re not imagining it. These heat surges aren’t just from the weather—they’re hormonal, and they can hit hard. The classic symptoms of perimenopause—hot flushes and night sweats—are well known. But many women also experience burning sensations in the feet or hands, skin sensitivity, and heat intolerance, especially during the summer months[1]. Why do we overheat during perimenopause? Oestrogen doesn’t just regulate your menstrual cycle—it helps manage body temperature, circulation, and mood. As levels start to fluctuate (often wildly) during perimenopause, your brain can misinterpret small changes as overheating. Cue: sweating, flushing, and restlessness[2]. What’s more, declining oestrogen affects the nervous system and skin, sometimes causing burning feet, tingling hands, or even electric shock–like sensations[3], less common but very real symptoms many women don’t expect. 6 Ways to keep cool, naturally 1. Hydrate intelligently Drink 1.5–2 litres of water daily, and add a pinch of sea salt or a splash of coconut water to restore electrolytes lost through sweating[8]. 2. Cool your feet Soak burning feet in cool (not icy) water with Epsom salts. The magnesium helps ease nerve irritation and relax tense muscles[9]. 3. Wear breathable fabrics Choose loose-fitting clothes made from cotton, bamboo or linen. Avoid synthetic materials which trap heat and can irritate sensitive skin. 4. Use cooling herbs Sage tea, peppermint, red clover, and evening primrose oil have shown promise in reducing hot flushes and night sweats[10]. 5. Prioritise sleep Keep your bedroom cool, dark, and quiet. Try sleeping with a fan, and avoid screens an hour before bed to support natural melatonin production[11]. 6. Mindful movement & rest Exercise helps regulate temperature and stress, but overdoing it can backfire. Try gentle yoga, walking, or swimming, and listen to your body. Gut Health: The foundation of menopause symptom relief When it comes to managing perimenopausal symptoms, whether it’s hot flushes, burning feet, mood swings or sleep disruption, your gut health should be the first place you start when looking to manage your symptoms. Think of it as the foundation of your menopause toolkit. Whether you’re taking HRT or not, a healthy gut sets the stage for better hormonal balance, stronger immunity, and a calmer nervous system[4]. It also helps to: 1. Regulate oestrogen levels naturally Certain gut bacteria, often referred to as the estrobolome, help break down and recycle oestrogen in the body. A balanced gut microbiome means fewer hormonal highs and lows, which can reduce hot flushes, mood dips, and more[5]. 2. Reduce systemic inflammation Chronic inflammation, often driven by gut imbalances, can heighten symptoms like burning skin, joint pain, or general heat sensitivity[6]. By supporting your gut, you’re helping your entire system stay calmer and more resilient. 3. Improve sleep, mood & stress response The gut-brain axis directly affects how well you sleep, how stressed you feel, and how your nervous system responds to temperature and discomfort. A healthy gut helps modulate cortisol (stress hormone) and supports production of mood-stabilising serotonin[7] Feed your gut (with targeted support for women in perimenopause) Gut health is foundational, but not all probiotics are created equal. If you're in your 40s or 50s and navigating perimenopause, supporting your gut with targeted probiotic strains is one of the most effective steps you can take. Why a targeted probiotic like Better Gut matters: Aids in oestrogen metabolism for fewer hormonal spikes Reduces bloating and gut sensitivity often triggered by stress and food changes Supports immune balance, which is crucial as hormone levels shift Helps calm burning sensations and flushes from the inside out Pair with a fibre-rich, gut-loving diet: Eat prebiotic foods like leeks, asparagus, bananas, and oats Include fermented foods (as tolerated) such as kefir or sauerkraut Stay hydrated with water, herbal teas, and mineral-rich broths Final thoughts: Thriving, not just surviving Perimenopause is a natural phase of life, not a medical condition, but that doesn’t mean you have to suffer through it. Whether it’s blazing hot outside or your internal thermostat is having a moment, you can take back control with simple, science-backed strategies. Start with your gut. Support it daily with targeted probiotics and nourishing foods. Hydrate. Cool down. And most importantly, listen to your body with compassion. You’re not just powering through—you’re creating a foundation for the next vibrant chapter of life. References NHS. Menopause symptoms British Menopause Society. Guidance on menopausal symptoms Women's Health Concern. Menopause Fact Sheet National Institutes of Health (NIH). Gut microbiota and menopause: A review Plottel, CS et al. "The human microbiome and estrogen metabolism." Cell Press, Trends in Endocrinology & Metabolism. Cani, PD. "Gut microbiota and inflammation." Current Opinion in Clinical Nutrition, 2011. Mayer, EA. "Gut/brain axis and the microbiota." Journal of Clinical Investigation, 2015. EFSA (European Food Safety Authority). Hydration guidelines NIH. Magnesium: Fact Sheet for Health Professionals. NIH Magnesium National Center for Complementary and Integrative Health. Herbs and Supplements Sleep Foundation. Menopause and Sleep
Read moreBerberine and menopause: A natural ally for weight management
A Natural Way to Support a Healthy Metabolism There’s growing interest in new approaches to weight management, especially those focused on metabolic health and appetite regulation. While some prescription options have made headlines, they often come with side effects and may not offer lasting support once use is discontinued. For those looking for a more natural approach, there’s Berberine, a powerful botanical compound with a long history of traditional use and growing scientific interest. It’s the hero ingredient in our new formula, Better Metabolism. Berberine has been studied for its potential to: Support healthy blood sugar levels already in the normal range Promote energy production Support metabolic function, particularly during midlife These benefits make it a compelling option for those navigating the changes that come with perimenopause and beyond. If you're looking for a gentle, sustainable way to support your metabolism—without harsh stimulants or prescriptions—Berberine could be a valuable tool in your wellness routine. Berberine: Nature’s metabolism ally Berberine has been used for thousands of years in traditional Chinese and Ayurvedic medicine, and modern science now supports its impressive range of benefits. It’s been shown to: Improve insulin sensitivity[2] Lower fasting blood glucose and HbA1c levels[3] Regulate lipid metabolism and reduce triglycerides[4] Activate AMP-activated protein kinase (AMPK) – your body’s metabolic switch[5] Support weight management in insulin-resistant individuals[6] AMPK is the same enzyme activated by exercise and fasting. It tells your cells to shift from “store fat” mode into “burn energy” mode, helping support healthy glucose levels, fat metabolism, and even mitochondrial function. Why we created Better Metabolism At The Better Menopause, we know that midlife metabolic shifts aren’t just about weight, they’re about energy, blood sugar, gut health, and inflammation. That’s why Better Metabolism has been formulated with a blend of complementary high-strength ingredients, including: Berberine – Supports glucose control and AMPK activation Cinnamon extract – Enhances insulin signalling and reduces post-meal blood sugar spikes[7] Chromium – Aids in glucose transport and helps curb sugar cravings[8] Myo-Inositol – Enhances insulin function and supports hormone balance, particularly in PCOS[11 What about your gut health? Berberine doesn’t just support metabolism, it may also play a key role in gut health. Thanks to its natural antimicrobial properties and it’s been used in functional medicine for gut imbalances like SIBO (small intestinal bacterial overgrowth). Early research shows Berberine may actually support the growth of beneficial bacteria, including Akkermansia muciniphila, which is linked to improved metabolic function and gut barrier integrity.[12] To enhance this effect, we recommend pairing Better Metabolism with our targeted gut formula, Better Gut, a targeted probiotic of clinically backed bacterial strains, formulated to rebalance the microbiome and support gut lining integrity during perimenopause and beyond Together, they form a powerful duo for women navigating the metabolic and digestive shifts of midlife. Discover our Body Bundle here Final Thoughts: not a quick fix, a smarter long-term strategy For women in erimenopause and menopause looking to regain balance, Better Metabolism offers a researched, well-rounded solution that supports energy, blood sugar, and fat metabolism, without extreme pharmaceutical intervention for sustained weight management. References Nauck MA, Meier JJ. “Management of endocrine disease: Are all GLP-1 agonists equal in the treatment of Type 2 Diabetes?” Eur J Endocrinol. 2019;181:R211–R234. Chang W, Hatch GM, et al. “Berberine as a therapy for type 2 diabetes and its complications.” Biochem Cell Biol. 2015 Oct;93(5):479-86. Dong H, Wang N, Zhao L, Lu F. “Berberine in the treatment of type 2 diabetes mellitus: a systemic review and meta-analysis.” Evid Based Complement Alternat Med. 2012;2012:591654. Kong W, Wei J, Abidi P, et al. “Berberine is a novel cholesterol-lowering drug working through a unique mechanism.” Nat Med. 2004;10(12):1344-1351. Francini F, Schinella GR, Ríos JL. “Activation of AMPK by Medicinal Plants and Natural Products.” Mini Rev Med Chem. 2019;19(11):880–901. Yin J, Xing H, Ye J. “Efficacy of berberine in patients with type 2 diabetes mellitus.” Metabolism. 2008;57(5):712-717. Cao H, et al. “Anti-diabetic effect of cinnamon: implications for its use in prevention and treatment of Type 2 Diabetes.” Nutr Res Pract. 2007. Anderson RA. “Chromium, glucose intolerance and diabetes.” J Am Coll Nutr. 1998;17(6):548-555. Packer L, Witt EH, Tritschler HJ. “Alpha-lipoic acid as a biological antioxidant.” Free Radic Biol Med. 1995;19(2):227-250. Malaguarnera M. “Carnitine derivatives: clinical usefulness.” Curr Opin Gastroenterol. 2012 Mar;28(2):166–76. Nestler JE, Jakubowicz DJ, et al. “Effects of inositol on ovarian function in women with PCOS.” N Engl J Med. 1999. Dong C, Yu J, Yang Y, et al. “Berberine, a potential prebiotic to indirectly promote Akkermansia growth through stimulating gut mucin secretion.” Biomedicine & Pharmacotherapy. 2021;139:111595.
Read moreMenopause and sleep: 6 natural ways to beat 3am wake-ups
Struggling with restless nights, 3am wake-ups, or that frustrating ‘wired but tired’ feeling? You’re not imagining it—and you’re definitely not alone. Many women going through perimenopause and menopause experience disrupted sleep due to hormonal changes, elevated stress, and imbalances in gut health. In this expert-backed guide, discover the root causes of menopause-related insomnia—and six proven, natural strategies to help you sleep more deeply and wake up refreshed. Why menopause disrupts your sleep 1. Hormonal Fluctuations As oestrogen and progesterone decline during perimenopause and menopause: Oestrogen helps regulate your internal clock and body temperature. Lower levels can trigger hot flushes and night sweats that disturb sleep. Progesterone is a calming hormone that promotes rest. When it drops, sleep becomes lighter and more fragmented. 2. Elevated cortisol at night Hormonal changes and midlife stressors can lead to higher cortisol levels in the evening—making it harder to relax, fall asleep, or stay asleep. 3. Gut health disruptions Your gut plays a crucial role in producing serotonin, which converts to melatonin—your body’s natural sleep hormone. When your microbiome is out of balance, so is your sleep cycle. 6 natural ways to sleep better during menopause 1. Lower cortisol with an evening wind-down Practise mindfulness or deep breathing Try restorative yoga or gentle stretching Limit screens for at least 60 minutes before bed 2. Create a sleep-optimised bedroom Keep your room cool, dark, and quiet Use blackout blinds and natural, breathable bedding Dim lights and reduce blue light exposure in the evening 3. Move daily—but time it right Regular physical activity supports better sleep, but avoid high-intensity workouts after 6pm as they can spike cortisol. Try walking, Pilates, or swimming earlier in the day. 4. Support your gut for better sleep Since your gut produces serotonin and influences melatonin, nurturing your microbiome can significantly improve sleep quality, especially in perimenopause when hormone fluctutaions disrupt the delicate balance of tour gut microbiome. Better Gut is a daily probiotic designed to support digestion, mood, and sleep. It includes 6 clinically studied strains such as Lactobacillus rhamnosus and Bifidobacterium lactis, which help reduce cortisol and promote a balanced microbiome. 5. Nourish your nervous system naturally Hormonal stress can deplete key nutrients that your body needs to relax and recover overnight. Better Night is a gentle, non-habit-forming supplement formulated to help you fall asleep faster, stay asleep longer, and feel clear-headed in the morning. It includes KSM-66® Ashwagandha, Affron® Saffron, Chamomile, Magnesium, Montmorency Cherry, and essential vitamins B6, B12, D3, and K2. 6. Try mind–body therapies Use guided meditation or body scans before bed Keep a gratitude journal to unwind your thoughts Experiment with calming sounds, breathing exercises, or visualisations Support your sleep from the inside out If you’re ready to address the root causes of menopause-related sleep issues—like gut health, cortisol balance, and hormonal shifts—consider pairing Better Gut and Better Night. Our Better Bundle gives you both formulas in one easy routine, so you can: Balance your gut microbiome Lower night-time cortisol Support your natural sleep–wake rhythm Because better nights mean better days. And you deserve both. References NIH – Sleep and Hormone Fluctuations in Menopause NIH – Effects of Stress on Sleep and Cortisol NIH – Gut Microbiota and Sleep Regulation NHS – Exercise and Sleep
Read moreCortisol, gut health & menopause: What you need to know
Menopause is a natural transition—but let’s be honest, it doesn’t always feel natural. If you're experiencing fatigue, mood swings, weight gain, brain fog, or sleep issues, you’re not alone. While hormone changes often take the blame, there’s another overlooked culprit: cortisol, your body’s primary stress hormone. What many women don’t realise is how closely cortisol is connected to gut health. This connection influences everything from your mood to your metabolism—and is the reason why many women are turning to targeted gut-supporting supplements like Better Gut to naturally reduce stress and ease menopause symptoms. What is cortisol—and why it matters during menopause Cortisol is produced by your adrenal glands in response to stress. It’s essential for regulating: Your sleep–wake cycle Blood sugar and metabolism Inflammation and immune response Fat storage and energy use However, during menopause, reduced levels of oestrogen and progesterone can make the body more sensitive to cortisol—leading to stronger and longer-lasting stress responses. [1] How high cortisol levels worsen menopause symptoms Hot flushes & night Sweats Cortisol interferes with your hypothalamus, the part of the brain that regulates temperature. This may contribute to the sudden heat surges and night sweats many women experience in menopause. [2] Insomnia & sleep disruption At night, cortisol should naturally drop. But under stress, it can remain elevated—making it difficult to fall asleep or leading to 2–3 a.m. wake-ups. Supporting your nervous system with calming nutrients like ashwagandha, magnesium and vitamin B6—as found in Better Night—can help restore your natural sleep cycle. [3] Mood Swings, anxiety & brain Fog Elevated cortisol can disrupt neurotransmitters in your brain, making it harder to regulate mood and memory. Ingredients like affron® saffron, ashwagandha, and GABA-supportive B vitamins have been shown to ease stress and support mood stability—making targeted support like Better Night a smart addition to your routine. [4] Weight Gain, especially around the middle Cortisol tells your body to store belly fat and triggers cravings for high-sugar, high-fat foods. A healthy gut can help balance these cravings by improving blood sugar regulation and nutrient absorption. [5] Bloating, food sensitivities & inflammation Cortisol compromises your gut lining and microbiome diversity, contributing to systemic inflammation. A high-quality probiotic—like Better Gut—can help repair this balance, supporting digestion and reducing inflammatory symptoms. [6] The gut–cortisol–menopause feedback loop Stress raises cortisol, which damages the gut, leading to inflammation and worsened hormone symptoms—creating a loop that’s hard to break. But research shows that targeting the gut–hormone–stress axis can reduce symptoms holistically. Stress → High Cortisol → Gut Imbalance → More Inflammation → More Symptoms → More Stress This is exactly why many women start by improving their gut health when looking for long-term menopause relief. The role of gut health during menopause There’s a profound connection between your gut and your hormones during menopause. Flutuating hormones disrupt the delicate balance of the gut microbiome leading to a range of symptoms—including bloating, mood swings, brain fog and hot flushes—supporting your gut during this time woth tailored probiotic can help reduce your symtoms as well as helping regulate cortisol, balance oestrogen, and reduce inflammation. Better Gut is a high-strength probiotic supplement formulated with 50 billion CFUs and six targeted bacterial strains selected to support gut and hormone health during perimenopause and menopause. Each strain was chosen for its specific benefits in relieving common menopause symptoms: Lactobacillus rhamnosus – Can help improve stress resilience, reduce anxiety, and ease bloating, inflammation, and vaginal dryness HOWARU® Lactobacillus rhamnosus – A clinically studied strain shown to reduce stress and support emotional wellbeing Lactobacillus acidophilus – Helps protect against vaginal and urinary tract infections by maintaining a healthy vaginal microbiome Bifidobacterium lactis – May help reduce the severity and frequency of hot flushes and night sweats Lactobacillus reuteri – Supports mood balance and sleep quality Bifidobacterium bifidum – Promotes healthy digestion and regularity, helping to relieve menopause-related constipation This targeted blend works in harmony with your body to help restore balance from within—supporting digestion, stress regulation and hormonal health during every stage of menopause. Shop Better Gut and use code WELCOME15 for 15% off your first order. Evening support: How Better Night helps to regulate cortisol Quite often high cortisol levels result in middle of the night wake-up, that's where a adaptogens like Ashwagandha can really support you. Better Night is a non-sedating, hormone-friendly formula designed to support natural sleep cycles disrupted by cortisol. It combines: KSM-66® Ashwagandha – Clinically shown to reduce cortisol and improve sleep quality Affron® Saffron – Improves mood and emotional regulation at night Magnesium Glycinate – A highly absorbable form for calming nerves and muscles Chamomile & Vitamin B6 – To relax the body and support melatonin production These ingredients are ideal for supporting deep, restorative sleep—without next-day grogginess. Try Better Night to wind down, stay asleep, and support your emotional health overnight. Additional lifestyle strategies to naturally lower cortisol In addition to targeted supplements like Better Gut and Better Night, daily habits play a big role in regulating cortisol levels. Here are simple, sustainable strategies that can help support your stress response: Practice daily mindfulness – Just 10 minutes of deep breathing, meditation, or yoga can lower cortisol and improve mental clarity. Prioritise gentle movement – Swap intense workouts for walks, Pilates or tai chi. Overtraining can actually raise cortisol. Eat regular, balanced meals – Skipping meals or restricting carbs can spike cortisol. Include whole grains, lean protein, and healthy fats at each meal. Cut back on caffeine and alcohol – Both can disrupt sleep and elevate cortisol, especially in the evening. Get sunlight exposure in the morning – Helps regulate your circadian rhythm and promotes healthy cortisol patterns. Set consistent sleep and wake times – A regular sleep routine is one of the most effective ways to support hormone balance and reduce stress reactivity. Journal or reflect before bed – Offloading worries in a notebook can quiet your mind and help you sleep more deeply. These lifestyle changes, when paired with targeted support like Better Gut and Better Night, create a solid foundation for navigating menopause with more energy, better sleep, and fewer stress-driven symptoms. Menopause doesn’t have to feel out of control If you’re feeling out of balance, your gut and stress hormones may be to blame. By restoring your gut health and managing cortisol naturally, you can begin to ease symptoms—from sleep issues to mood swings—without relying solely on short-term fixes. Start by giving your body what it needs to self-regulate. Explore our Better Bundle to support your menopause, naturally. References Menopause and the HPA Axis – Otte et al., 2005 Pathophysiology of Menopausal Hot Flushes – Freedman, 2005 Sleep Loss and Elevated Cortisol – Leproult & Van Cauter, 1997 Stress and Brain Function – Lupien et al., 2009 Stress and Body Shape – Epel et al., 2000 Stress and the Gut–Hormone Connection – Chrousos, 2000
Read moreWhy do random chin hairs appear after 40? The surprising truth
You’re casually checking the mirror when, bam! a rogue chin hair appears out of nowhere. If you’ve noticed random chin hairs popping up after 40, you’re not alone. Many women experience these pesky strays, often wondering, Where did that come from? And why does it feel like steel wire?! This article explores the hormonal causes behind post-40 facial hair, why it happens during perimenopause and menopause, and - most importantly - how to manage it safely and effectively. Why do chin hairs appear after 40? The culprit? Hormonal changes. As women enter perimenopause (late 30s to early 40s) and menopause (typically 45+), their oestrogen levels decline, while testosterone remains stable or even increases proportionally. This shift can lead to: ✔ Thicker, darker facial hairs (hirsutism) ✔ A decrease in collagen and skin elasticity(making hair more noticeable) ✔ Faster-growing coarse hairs on the chin, jawline, and upper lip According to the NHS, menopause-related hormonal shifts can affect everything from hair growth to metabolism, leading to noticeable changes in facial hair. The role of hormones: oestrogen vs. testosterone Before 40: Oestrogen keeps testosterone in check, preventing excess hair growth. After 40: With less oestrogen, testosterone has a greater influence, leading to the emergence of random facial hairs This is why some women never had facial hair in their 20s but suddenly find themselves tweezing chin hairs at 45. Other factors that contribute to chin hair growth Besides hormonal changes, other factors can cause those stubborn chin hairs to sprout: Genetics – If your mum or grandmother had chin hairs, you might, too. Polycystic Ovary Syndrome (PCOS) – A common condition causing excess androgens. Stress & Cortisol – High stress levels can impact hormone balance and increase hair growth. Medications – Some drugs (e.g., steroids, hormone therapies) may trigger facial hair. The British Menopause Society notes that changes in hormone levels during menopause may contribute to increased facial hair growth in women. How to get rid of chin hairs (safely & effectively) If the occasional rogue hair doesn’t bother you, that’s perfectly fine! But if you prefer smoother skin, here are some safe removal options: Quick Fixes: Tweezing – Best for a few stray hairs; results last 2-4 weeks. Dermaplaning – Removes fine peach fuzz + exfoliates skin. Longer-Term Solutions: Waxing or Threading – Lasts 4-6 weeks but may cause irritation. Laser Hair Removal – Reduces growth over time (best for darker hairs). Electrolysis – Permanent hair removal by destroying hair follicles. Can probiotics help reduce chin hair growth? Emerging research suggests that probiotics may play a role in balancing hormones during menopause, which could indirectly help reduce unwanted facial hair Menopause disrupts the gut microbiome, affecting hormone metabolism—particularly oestrogen and androgens (like testosterone). Certain probiotic strains, such as Lactobacillus and Bifidobacterium, have been studied for their ability to: Support hormonal balance– Helping regulate oestrogen metabolism, which may prevent excessive androgens from triggering facial hair growth. Improve insulin sensitivity – Studies show that hormonal imbalances and insulin resistance are linked to excess hair growth (hirsutism) in some women. Probiotics may help stabilise blood sugar, reducing excess androgens Reduce inflammation – A healthy gut can help reduce inflammation-related stress on hair follicles, which may contribute to hair thinning or excess growth. How can probiotics help? If you’re looking for natural ways to support hormonal balance, a high-quality menopause-specific probiotic supplement may be beneficial. Look for clinically studied probiotic strains like those in the Better Gut probiotic. Support with a balanced diet rich in fibre, fermented foods, and hormone-friendly nutrients. While probiotics won’t remove chin hairs overnight, they can support your body’s natural hormone regulation, making them a complementary option alongside other treatments. Want to learn more? Explore our probiotic formula for menopause here. When to See a Doctor If chin hair growth is sudden, excessive, or accompanied by other symptoms (like irregular periods, weight gain, or acne), it may signal an underlying condition like PCOS or adrenal issues. A doctor can check hormone levels and recommend treatments. Final Thoughts Random chin hairs after 40 are a natural part of ageing and hormonal shifts, but they don’t have to be a nuisance. Understanding why they appear and knowing how to manage them can make the process a little less annoying. References: 1. NHS – Menopause and Hormone Changes. (Accessed: March 2024) https://www.nhs.uk/conditions/menopause/ 2. British Menopause Society – Hirsutism in Menopause. (Accessed: March 2024) https://thebms.org.uk/ 3. Probiotics and Hormonal Balance in Menopause: A Review. (2021) [https://pubmed.ncbi.nlm.nih.gov/34109594
Read moreSaffron for Menopause Relief: A Natural Way to Support Mood, Sleep & Libido
For many women in their 40s and 50s, perimenopause and menopause can feel like an emotional and physical upheaval. Mood swings, anxiety, disrupted sleep, low libido, and hot flushes are all too common. While hormone replacement therapy (HRT) and antidepressants are often prescribed, a growing number of women are seeking natural, evidence-based solutions to support their wellbeing during this life stage. One promising option is saffron – not just a culinary spice, but a clinically researched botanical that has shown real benefits for mood, sleep, and emotional balance. A patented extract called Affron® has been the focus of multiple human studies and is featured at the full clinical dose of 30 mg in our supplement, Better Night™ – a natural sleep and stress formula designed specifically for women in midlife. Why Saffron? Saffron (Crocus sativus) contains active compounds like crocin and safranal, which influence key brain chemicals involved in mood regulation – including serotonin, dopamine, and norepinephrine. These neurotransmitters are often impacted during perimenopause and menopause, contributing to anxiety, low mood, and irritability. Saffron works by gently supporting this neurochemical balance, without acting as a hormone. Unlike phytoestrogens or synthetic hormones, saffron does not mimic oestrogen or disrupt endocrine function. This makes it a safe and versatile option, especially for women who cannot or choose not to take HRT. Backed by Clinical Research One of the largest menopause-focused studies on saffron involved 86 women aged 40 to 60 who took 28 mg of Affron® saffron extract daily for 12 weeks. According to the results published in the Journal of Menopausal Medicine, participants experienced: A 33% reduction in anxiety symptoms A 32% reduction in depressive symptoms Significant improvement in emotional wellbeing without any major side effects Read the study summary here. Better Night™ contains 30 mg of Affron® – slightly more than the clinically studied dose – to ensure full support for mood balance, calm, and mental clarity during perimenopause. Sleep Support Without Hormones Insomnia and sleep disturbances are among the most frustrating menopause symptoms. Night sweats, stress, and shifting hormones can make restful sleep elusive. Fortunately, saffron has also been shown to help improve sleep quality in several studies. In a placebo-controlled trial involving adults with poor sleep, both 14 mg and 28 mg of Affron® saffron taken daily improved: Sleep latency (falling asleep faster) Sleep duration Morning energy and alertness View the full study results here. Better Night™ includes 30 mg of Affron® to help you fall asleep more easily, sleep more deeply, and wake up feeling rested. Libido and Intimacy A decline in sexual desire is another common (and often distressing) symptom of menopause. Stress, fatigue, low mood, and hormonal shifts can all dampen libido. Saffron, traditionally used as an aphrodisiac, is now supported by modern science for its role in improving sexual function in women. In a clinical trial, women taking 30 mg of saffron daily for 6 weeks experienced: 62% improvement in their Female Sexual Function Index (FSFI) scores Greater desire, arousal, lubrication, and satisfaction Read the full trial on PubMed. Better Night™ supports libido both indirectly through mood and stress support, and potentially directly through saffron’s role in supporting pleasure-related neurotransmitters like dopamine. What About Hot Flushes? Although saffron is not a direct treatment for hot flushes, it may help by calming the nervous system and reducing the anxiety and stress that often intensify them. Since hot flushes can be triggered by emotional stress or disrupted sleep, saffron’s mood-stabilising and sleep-supporting effects can make them less frequent or easier to manage. Some women who use Better Night™ report that while their flushes haven't disappeared entirely, they feel more resilient and less reactive, thanks to better emotional regulation and more consistent rest. Why Choose Better Night? Better Night is uniquely formulated for women navigating the menopause transition, offering: 30 mg of clinically studied Affron® saffron extract A non-hormonal, non-sedative formula Support for mood, sleep, stress, and libido A trusted, natural solution backed by science Shop Better Night now. The Takeaway Perimenopause and menopause don’t have to mean giving up on restful sleep, emotional balance, or intimacy. Nature provides options – and saffron, especially the clinically tested Affron® extract, is one of the most promising. Better Night™ combines the full clinical dose of Affron® (30 mg) in a simple daily capsule, supporting better sleep, improved mood, and enhanced resilience during the menopause transition – without the use of hormones or harsh medications. Explore Better Night today and discover a natural way to restore calm, clarity, and comfort during midlife. References Lopresti, A. L., & Smith, S. J. (2021). The effects of a saffron extract (Affron®) on menopausal symptoms in women during perimenopause. NutraIngredients. Lopresti, A. L., et al. (2020). Effects of saffron on sleep quality in healthy adults. NeurologyLive. Kashani, L., et al. (2022). Crocus sativus (saffron) in the treatment of female sexual dysfunction. PubMed. Montemarano, M. (2021). Saffron extract may help menopause symptoms. Nutraceuticals World. Psychiatric Times (2019). Is there a role for saffron phytotherapy in treating depression? Psychiatric Times.
Read moreWinter Hormone Health: Top Ten Tips for Supporting Your Well-being
As the New Year begins, it’s the perfect time to focus on your health and set a strong foundation for the months ahead.
Read moreThe Top 10 Nutritional Benefits of a Traditional Christmas Dinner for Women’s Health
A traditional Christmas dinner isn’t just a festive indulgence; it’s a meal brimming with nutrients that can support women’s health, particularly during perimenopause.
Read moreHow menopause affects metabolism and how to improve yours
What is metabolism, how is it affected by menopause and how can you boost yours to improve your health?
Read moreUnderstanding menopause weight gain
Hormone changes, muscle loss and poor sleep can lead to weight gain and increased belly fat during perimenopause and menopause – but there are things you can do to manage it.
Read moreLifestyle tips for losing weight during menopause – and keeping it off
How to support sustainable weight loss during menopause – what to eat, what to limit, the best forms of exercise and tips for better sleep.
Read moreThe links between menopause and leg pain, and the approaches that could help
What does menopause leg pain feel like, what’s the link to changing hormone levels and what could help ease your symptoms?
Read moreImproving your diet for healthy menopause weight loss
Discover the dietary changes you can make to lose menopause weight and belly fat in a sustainable and healthy way, and get inspiration planning your meals.
Read moreNatural supplements that may help with menopause weight loss
We assess the evidence that these natural supplements could aid weight loss and reduce belly fat during menopause, and look at what else you can do to maintain a healthy weight.
Read moreWhat causes menopause brain fog and what can you do about it?
Discover the links between menopause, hormones and brain fog, how long it lasts and the treatments, supplements and lifestyle changes that could help.
Read moreCan your GP prescribe testosterone for menopause?
Learn why testosterone is unlicensed for women in the UK, when it can be prescribed on the NHS, how to get a private prescription and where you can buy testosterone.
Read moreWhy testosterone is important for women and how it could help during menopause
Discover why your body needs testosterone, how testosterone therapy could help during menopause and where you can get it.
Read moreWhat’s causing your burning feet during menopause, and what could help?
Exploring the links between menopause, hormone changes, vitamin deficiencies and hot or burning feet, plus the treatments that could improve your symptoms.
Read moreMedication, supplements and tips to boost your sex drive during menopause
How menopause affects your sex drive and sexual health, and what you can do to increase your libido and make sex more pleasurable.
Read moreHow vitamin D can help with menopause
Everything you need to know about vitamin D and menopause, including the causes and signs of vitamin D deficiency, the best types, how much to take and the symptoms it can help with.
Read moreHRT alternatives and complementary approaches
Learn about the herbal blends, probiotics, lifestyle changes and other prescription drugs that could help with menopause symptoms as an alternative to HRT, or alongside it.
Read moreHow does menopause effect ADHD and could it lead to a diagnosis?
Discover the links between menopause and ADHD, how hormone changes could lead to a diagnosis and what you can do to help relieve your symptoms.
Read moreUnderstanding menopause anxiety and natural ways to manage it
How to spot menopause anxiety, the role fluctuating hormones play, how long it could last, where HRT comes in and some natural ways to manage it.
Read moreMenopause burning mouth, dry mouth, sores and ulcers
Learn about the possible causes of burning mouth syndrome during menopause, the links to other oral health conditions and what can you do to treat your symptoms.
Read moreWhy your body odour could change during menopause, and what you can do about it
Exploring the hormone changes and other factors that can affect body odour during perimenopause and menopause and what you can do to manage it.
Read moreWhat Happens to Your Period During Perimenopause?
Thought you knew exactly where you were with your cycle, until all of a sudden everything changed? Erratic periods, heavy flow, longer cycles, shorter cycles… The possibilities are endless when it comes to perimenopause! So what exactly happens to your period during this time, and what can you do to manage the uncertainty of it all? Award winning GenM (and menopause friendly!) period brand, WUKA, explains more. What is Perimenopause? Most of us learned about the first period at school, but nobody really about the last period, let alone what happens to your cycle in the lead up to that very last bleed. The transition from regular cycles to menopause is called Perimenopause, and thankfully the conversation surrounding it is starting to open up, and we’re starting to understand more about what happens during this time. For some, perimenopause can last up to 10 years, and the age at which it starts can vary form person to person too. What Happens During Perimenopause? During perimenopause the ovaries gradually begin to stop working. It’s a natural process that will happen to us all eventually, and it brings with it quite a range of symptoms, most common of which include: Hot flushes Night sweats Heavy periods Mood swings There are actually a range of other physical and emotional symptoms that can occur too- and changes to your period are, for many, a first sign that perimenopause has begun. Changes to Your Period Fluctuating hormones are at play here. So what can we expect? Shorter Cycles The slowing down of the ovaries can cause the follicular phase to become shorter, which in turn leads to early ovulation- and therefore a shorter cycle overall. Longer Cycles Just like above, longer cycles are also caused by fluctuating hormone levels, and your actual period could last longer than your usual 2-5 days too. Changes to your flow Lots of women going through perimenopause experience changes to their flow, again thanks to fluctuation of hormones. For many, the drop in progesterone can trigger heavy bleeding, and this is very common during the early stages of perimenopause. But just to make it interesting, some cycles may be lighter than usual, and others may be heavier (whilst also being shorter, then longer, then shorter again… ) - so just what is happening here? Hormones, hormones, hormones. As the ovaries slow down, they might not produce an egg for ovulation during some cycles. This is called an anovulatory cycle, and results in a lighter blood flow. When ovulation does occur, your period will be heavier- and if your cycle has been longer than normal, your flow could be heavier than normal too. Towards the end of perimenopause, fluctuations of hormones become a little more intense, and variations in your cycle can occur more and more. In other words, you might not know what’s happening or when! Managing Your Period During Perimenopause It’s not easy trying to predict how your cycle is going to behave from one month to the next, and if you’ve always been regular it can be quite frustrating too. So how do we manage our period with all of this uncertainty? Make the switch to period pants. Here are just three reasons why it’s a good idea: Leak-free confidence: When your flow is super heavy, the last thing you want is to spend half the day in the loo changing leaking pads or tampons. WUKA’s Super Heavy Flow period pants hold up to 60ml period blood, meaning you can wear them for longer without fear of leaks. Yes, even at nighttime. Thanks to an extra long gusset, these pants are guaranteed to hold it all in, all while keeping you feeling fresh and dry too. Just-in-case-reassurance: Erratic cycles can be hard to navigate, and nobody has the spare cash to waste on plastic-filled disposables that might or might not be needed. Luckily, period pants can be worn just like normal underwear, ready to absorb your flow if it decides to turn up. And if it doesn’t, just wash them with your normal laundry load and they’re ready to go for next time. Stay cool, stay comfy: Cycle changes aren’t the only symptom of perimenopause- temperature fluctuations, bloating, weight gain, cramps and vaginal dryness are all symptoms that could pop up as part of this journey towards menopause. And that’s on top of an erratic period! Don’t worry, WUKA period pants have got it covered. Their Stretch™ period pants feature CoolMax™ technology to keep you dry and fresh, and Stretch™ technology for a second-skin fit. This means that even if your flow is heavy, the blood will stay locked away from your body and you’ll stay comfy and odour-free. It also means that you’re guaranteed a perfect fit (each pair stretches up to 4 sizes) even if you’re bloated or you've gained some weight. No digging in and no chafing whatsoever- plus the Cotton Stretch™ period pants offer protection against irritation too. How to use period pants It’s never too late to make the switch to period pants, and they’re so easy to use. Wear like normal underwear, bleed into them, wash them. That’s it! After use, rinse in cold water as soon as you can, then wash as normal on a low heat setting (no hotter than 40 degrees), then either dry outdoors or inside on an airer. No fabric conditioner or tumble dryers. You’ll need around 5 pairs of pants per cycle- that’s one pair to wear, one pair for spare and one pair for nighttime, with two in the wash/ for extra heavy flow days. They’ll last up to two years if cared for properly, and can be used to absorb all the way from light flow (including spotting and/ or discharge) to super heavy flow. We also recommend WUKA DryTech™ reusable incontinence pants for lights leaks and dribbles (yet another delight of perimenopause- 1 in 3 women experience bladder weakness over the age of 35!). These pants also use their innovative Stretch™ technology so adjust up to 4 sizes in one pair. If you would like to try WUKA pants for your then head on over by clicking here and use code BETTERM10 for 10% off your first purchase.
Read moreWhat is restless legs syndrome and how is it linked to menopause?
Exploring the connection between restless legs syndrome and menopause, what it feels like and what you can do to relieve it.
Read moreMenopause mood changes and what you can do about them
Discover the links between menopause, perimenopause and mood symptoms, as well as the lifestyle changes, supplements and other treatments that could help.
Read moreHow menopause affects your sleep, and how you can improve it
Exploring the links between menopause, perimenopause and sleep problems, plus the natural remedies, treatments and supplements that could help.
Read moreNavigating HRT – Everything you need to know
Navigating HRT – Everything you need to know By Dr Rachel Hines Hormone replacement therapy (HRT) plays a vital role in managing menopause symptoms for many people, but it’s not for everyone. Some rave that it changed their life, others try it for six months but don’t get on with it. Some people never need or just don’t want it. Whether you're actively seeking help for your symptoms or just want to learn more about menopause, understanding how HRT works and who it can help is key. Here, we explore its benefits, when to consider it and treatment alternatives if it’s not for you. What is HRT? As the name suggests, hormone replacement therapy (HRT) is a kind of medication that supplies your body with hormones that are produced at lower levels during menopause. It has been consistently proven to be the most effective treatment for a range of menopause symptoms such as mood changes, hot flushes, painful sex and bladder symptoms. What are the different types of HRT? There are three different hormones you may need during menopause and two main types. Each hormone can also be taken in different ways, such as transdermally (through the skin) through a patch, cream or gel, or orally, as a tablet. Your doctor will help you decide which hormones and products are right for you. Here’s a summary of some of the options you may discuss. Oestrogen Menopause symptoms are mainly caused by fluctuating and declining oestrogen levels. Supplying your body with this hormone helps improve many menopause symptoms, which may include hot flashes, mood swings, vaginal dryness or trouble sleeping. Read more about the 34 symptoms of menopause. Progesterone Progesterone is prescribed alongside oestrogen if you still have your womb. When used alone, oestrogen can cause the lining of the womb to thicken, which increases the risk of developing womb cancer Thankfully, using progesterone alongside oestrogen removes this risk. Taking oestrogen and progesterone together is called combined HRT. Testosterone Testosterone is relatively new to the HRT scene. It is currently only prescribed for people who are stable on their systemic HRT (oestrogen with or without progesterone) and are still experiencing low libido. Read more about testosterone HRT. Systemic HRT This is HRT that is absorbed into the bloodstream and has effects across your body. This means it is used to treat body-wide - also known as systemic - menopause symptoms. Oestrogen, progesterone and testosterone can all be taken systemically. Vaginal oestrogen Vaginal HRT is applied inside your vagina - or to the wider genital area - and only works in the area where it is applied. It is a great option for people with vaginal, vulval or urinary symptoms, and can be used either alone or alongside systemic HRT. Vaginal HRT is always oestrogen only. Unlike other forms of oestrogen, you do not need to use progesterone if you’re taking vaginal oestrogen alone.There are quite a few more complexities to explore, but that covers the basics! When should you start HRT? There is no single answer to this question - we are all very different. Ultimately, it is your choice, and your doctor can help you make an informed decision once they are sure that menopause is behind your symptoms. Questions to consider together include: Are you open to hormonal treatment? Is HRT a safe option for you? How are your menopause symptoms impacting your life? And what does science say? It's best to start HRT within ten years of menopause and before the age of 60 to gain maximum cardiovascular benefits, according to research. Cardiovascular health relates to the health of the heart and blood vessels. Your doctor will usually advise you to start HRT straight away if you are diagnosed with premature ovarian insufficiency. Read more about when to start HRT. What are the risks and benefits of HRT? These will be different for everyone, as we all have a unique menopause experience and individual risk factors linked to our personal or family medical histories. The risks and benefits are also unique to the type of HRT you take. Benefits of HRT Menopause symptom relief is the main benefit of HRT. It is the most effective treatment for many menopause symptoms, including: Night sweats Hot flushes Mood changes, including low mood Sleep issues Genitourinary syndrome of menopause - this is an umbrella term for vaginal and urinary symptoms such as vaginal dryness, painful sex and frequent urination There are some other benefits too. HRT may also help: Protect the health of your bones, according to research Protect your heart and blood vessels- research suggests this happens if you start HRT within 10 years of menopause or before the age of 60 Reduce your risk of bowel cancer, as emerging evidence suggests Risks of HRT As with any medication, there are also risks to consider. These risks do not apply to all types of HRT and will be more or less important depending on your medical history. Increased risk of breast cancer. Oestrogen-only HRT - including vaginal HRT - causes little or no change to your risk of breast cancer. Combined HRT (oestrogen and progesterone) may increase your risk - about as much as drinking two or more units of alcohol per day, and not as much as being overweight. Increased risk of blood clots with oral HRT (tablets) Increased risk of stroke with oral HRT (tablets), more so when started in women over the age of 60 It is worth reading more about the benefits and risks of HRT to help inform your decision. There is still a lot for scientists to discover, but we know more now than ever before. Who can take HRT? You will be prescribed HRT if the benefits outweigh the risks for you personally. Due to the risks outlined above, doctors will not generally prescribe systemic HRT if you have any of the following: Breast cancer, whether past, present or suspected Known or suspected oestrogen-dependent cancers (meaning those which grow in response to oestrogen, most often in the breast, ovary, womb or endometrium) Certain types of arterial disease such as angina or heart attack Unexplained vaginal bleeding Untreated endometrial hyperplasia (abnormal thickening of the lining of the womb) Certain types of venous thromboembolism (blood clots) including pulmonary embolism (PE) and deep vein thrombosis (DVT), unless you are already on medications to thin the blood (anticoagulants) Thrombophilic disorders (conditions which increase your blood’s tendency to clot) Liver disease with abnormal blood tests Pregnancy Systemic HRT can sometimes be used for women with the above risk factors under specialist guidance. You may also still be able to take vaginal HRT even if you are not eligible for systemic treatment. There are a few other conditions and risk factors that may influence your doctor when prescribing HRT. Fortunately, there are other ways to treat and manage your menopause symptoms if HRT is not a safe recommendation for you. What can you do if you can't take HRT? Both non-hormonal medications and lifestyle changes can help manage common symptoms. Many people combine these approaches - sometimes it takes a bit of trial and error to find your most effective solution. Hot flushes Non-hormonal medications that can help hot flushes and other menopausal symptoms include: SSRI antidepressants, such as sertraline, citalopram or fluoxetine Clonidine Gabapentin Fezolinetant (Veozah) - a new medication now available in the UK on private prescription. Bladder and vaginal issues Vaginal oestrogen is the most effective treatment for the genitourinary syndrome of menopause (GSM), which includes symptoms like increased urinary frequency, vaginal dryness and painful sex. Itis generally safe to use, even if combined HRT is too risky for you. Non-hormonal options include: Vaginal moisturisers. These are widely available to help vaginal dryness or painful sex Lubricants. Try a pH-balanced lubricant to relieve painful sex Other symptoms Many lifestyle changes can have a huge impact on your menopause symptoms, including hot flashes, sleep issues, anxiety, bladder and vaginla symptoms and low mood. Try to: Get enough exercise Maintain a healthy weight Eat a nutritious diet Consider decreasing your caffeine, alcohol and/or nicotine intake Summary HRT may not be suitable for you because of your medical history or you may just prefer not to take it. That’s ok, HRT isn’t for everyone - there are alternative, non-hormonal medications and lifestyle change can make a real difference too. Your doctor will help you make an informed decision. If you would like to find out what your treatment options are, we have partnered with online menopause clinic, Stella, to give you access to their tailored menopause care. With Stella, you can skip NHS waiting times and talk to a doctor who has additional training in women’s health within a week. They will explain your options and if HRT is suitable, then send it to you in the post. You also get access to the Stella menopause app, where you can follow self-guided lifestyle change plans, speak to a real-life coach and try menopause-friendly workouts and recipes. All this for just £135. Take Stella’s assesment today. About the author Dr Rachel Hines Clinical Director of Menopause Services at Stella Dr Rachel is a GP and expert in menopause health. She has completed advanced menopause training with the Faculty of Sexual and Reproductive Healthcare and is on the British Menopause Society specialist register. She also has diplomas in sexual and reproductive healthcare, gynaecology and child health, and has specialised in women’s health throughout her career.
Read moreWhat causes menopause fatigue and what can you do about it?
From low energy to crashing fatigue, menopausal hormone changes could be causing your tiredness. Discover how the two are linked and what you can do to improve things.
Read more10 ways to tackle your menopause anxiety
We assess herbal remedies, supplements, lifestyle changes and other treatments that may help with anxiety during perimenopause and menopause.
Read moreNatural remedies for menopause mood swings and low mood
Experiencing irritability, mood swings or low mood? These herbal remedies, probiotic supplements, mindfulness approaches and lifestyle tips could help.
Read moreDoes menopause cause constipation, and what can you do?
Discover the connections between fluctuating hormones and constipation, plus the natural remedies, lifestyle changes and treatments that can help.
Read moreHerbal remedies, supplements and tips for better sleep during menopause
We look at six traditional herbal remedies that may improve your menopause insomnia, as well as other supplements and lifestyle changes that could help.
Read moreHow magnesium could help with your menopause symptoms
What does the science say about magnesium’s effects on menopause symptoms like sleep, anxiety and bone density, and which type of magnesium is best?
Read moreHow ashwagandha could help with your menopause symptoms
Scientists are studying this ancient herbal remedy for its potential benefits for sleep, mood, anxiety, brain fog and hot flashes.
Read moreThe early signs of perimenopause and what age to expect it
What are the early signs of perimenopause, what age does it happen, how long does it last, is there a test for it and how do you know when you've reached menopause?
Read moreHave you started perimenopause? See our checklist of symptoms
A checklist of 49 symptoms, as well as a printable symptom tracker to help you keep a record of your symptoms and monitor how they develop over time.
Read moreIs menopause causing your tingling extremities, and what can you do?
If you’re experiencing tingling, numbness or a feeling of ‘pins and needles’ in your hands, feet, limbs, face or body, it could be one of the less common symptoms of menopause. It’s called paraesthesia and for many women it seems to coincide with fluctuations in reproductive hormones like oestrogen during perimenopause – the transition to menopause. Although more research is needed, the link between perimenopause and paraesthesia may involve the roles these hormones play in nerve signalling and circulation around your body. Menopausal paraesthesia can be disconcerting and distracting, but for some women it’s also painful – more of a burning sensation than a tingling. Below, we’ll look more closely at paraesthesia symptoms and possible causes, as well as treatments and lifestyle changes that might improve things. If you also have other menopause symptoms, The Better Gut probiotic can help. This award-winning menopause supplement has been shown in scientific studies to reduce a whole range of symptoms, from hot flushes to digestive problems, anxiety to brain fog. To find out more visit Better Gut, where you can use the discount code WELCOME10 to get 10% off your first order. Do hormone changes during perimenopause and menopause cause paraesthesia? It’s not completely clear what causes paraesthesia during perimenopause and menopause and there’s currently not much research looking directly at whether it’s linked to hormone changes. However, fluctuating levels of oestrogen and progesterone do lead to a wide variety of other menopause symptoms, including hot flushes, brain fog and anxiety, and there are some reasons to think the same could be true of paraesthesia. One clue is the fact that some pre-menopausal women experience paraesthesia in the days before their periods – another time when hormones are in a state of flux and oestrogen levels are low. We also know that oestrogen plays a role in the functioning of the central nervous system, including how it communicates sensations around your body. It’s possible that changing levels of oestrogen during perimenopause could disrupt these signals, leading to unusual sensations. It may also partly explain why women can become more sensitive to pain during the menopause transition. Another symptom of menopause can be poorer circulation, particularly to your extremities. Anyone whose arm has ‘gone to sleep’ after they’ve leant on it for too long, will know that cutting off the circulation like this can lead to exactly the kind of numbness, followed by pins and needles, that some women experience during perimenopause. Still, more research is needed to confirm whether any of these factors do contribute to perimenopausal paraesthesia, and why some women experience it and others don’t. What does menopausal paraesthesia feel like? Although menopausal paraesthesia is most often described as a tingling feeling, you may experience any of a whole range of sensations in the affected areas. Some of the different ways women describe their paraesthesia include: tingling buzzing pins and needles prickling crawling static numbness stinging burning nerve pain electric shock You may also experience different sensations at different times, such as numbness followed by pins and needles. Where in your body can you get menopausal paraesthesia? Everyone’s experience of perimenopause and menopause is different and women report paraesthesia in a wide range of places around their bodies, including: hands and feet arms and legs face and head ears chest, torso or whole body Symptoms may change over time, moving from one place to another. You may also feel them in very specific areas, such as a particular numb spot. It’s important to be aware that paraesthesia can sometimes be a symptom of another health condition. See the section at the bottom of this article for more details and to find out when you should see a doctor. Tingling and numb hands and feet Tingling in your extremities, such as your hands and feet, is one of the most common forms of paraesthesia. It can often be felt as pins and needles and the areas can become numb. While not dangerous in itself, numbness in your feet could mean you’re more at risk of losing your balance and falling, while numb fingers and hands can make it hard to grip and to do things like type or write. Tingling face or head Your face is another common location for paraesthesia. You may feel it on just the lower part of your face, including your lips. It can sometimes feel as if there’s something on your face that you want to brush off. As well as a tingling sensation, paraesthesia around your head can be a pulsating feeling or involve sharp pains. Tingling ears If you’re experiencing tingling ears during perimenopause or after menopause, you’re not alone. Some women notice it specifically on their ear lobes, and even inside their ears. While this tingling sensation on your skin is not the same as tinnitus – a ‘phantom’ ringing sound in your ears – some women do experience the two together during perimenopause. Treatments and lifestyle changes that may help with paraesthesia Eating a balanced diet, exercising regularly and stopping smoking are some of the best things you can do for your overall health, and they may help with paraesthesia too. Hormone replacement therapy (HRT) may also be an option if your symptoms are caused by the menopause transition. A healthy diet A healthy, balanced diet will help to keep your nervous system functioning properly and could also reduce the severity of some menopause symptoms. To make sure you’re getting a wide range of nutrients, try to include as many different plants as possible – fruits and vegetables, beans and pulses, nuts and seeds. Choose wholegrains over highly processed options such as white rice and bread, and limit ultra-processed foods like packaged snacks and sugary drinks. Many plants contain compounds called phytoestrogens. These mimic some of the functions of oestrogen and may reduce certain menopausal symptoms. Beans and pulses, especially soyabeans, are a particularly good source of phytoestrogens called isoflavones. Regular exercise Regular exercise improves your circulation, which could help with numbness and pins and needles. It’s also been shown to reduce pain sensitivity and other menopause symptoms. The NHS and CDC recommend doing at least 150 minutes each week of moderate exercise, like brisk walking, or 75 minutes of intense exercise, such as running, spread over several days. You should also try to include a couple of sessions of strength work, such as weight training or bodyweight exercises. If you don’t currently do much exercise, start slowly and work your way towards these targets. Stopping smoking Just as exercise improves your circulation, smoking does the opposite, narrowing your blood vessels and reducing blood flow. In fact, just a single cigarette is enough to shut down the tiny blood vessels in one of your toes for up to three hours. Smoking can also increase your sensitivity to pain. While stopping smoking can be a challenge, the NHS and CDC offer plenty of help and support. Hormone replacement therapy HRT replaces the oestrogen and progesterone lost due to menopausal changes. Although it can help with lots of menopause symptoms, including hot flushes, mood swings and vaginal dryness, it doesn’t necessarily work for them all, or for everyone who tries it. There’s not much research looking at the impact of HRT on paraesthesia but, anecdotally, many women say it has reduced or got rid of their symptoms, while others say it hasn’t helped. If you’re thinking about trying HRT, talk to your doctor about whether it’s right for you and which treatment is the best option. Other causes of paraesthesia and when to see a doctor If you regularly have paraesthesia or numbness, and it’s not due to menopause, there are other medical conditions that could be causing it. These include: Diabetes: you may experience pins and needles or numbness in your hands and feet Raynaud’s: this circulatory disease can also cause your fingers or toes to change colour Sciatica: when your sciatic nerve is compressed, it can cause pain and pins and needles from your back, down your leg and into your foot Multiple sclerosis: numbness or tingling sensations can also be accompanied by muscle stiffness and spasms, fatigue and problems with balance, thinking and vision Shingles: this disease caused by the chickenpox virus leads to a painful rash on one side of your body that can begin with a tingling feeling Carpal tunnel syndrome: this problem with pressure on the nerve in your wrist can cause tingling, numbness and pain in your fingers Nerve damage or a trapped nerve Migraines Stroke or transient ischemic attack/’mini stroke’ Thyroid problems Don’t try to diagnose the problem yourself – if you have any of these issues, contact your doctor. Pins and needles can also have other causes, including: drinking too much alcohol poor diet poisonous substances certain medications medical treatments, such as chemotherapy abnormal levels of calcium, potassium or sodium vitamin B deficiency insect or spider bites seafood toxins If you regularly have paraesthesia or pins and needles, or it keeps coming back, you should talk to your doctor. Summary Paraesthesia is a tingling, crawling or burning sensation in your hands, feet, face, limbs or body. Although it’s not one of the most common symptoms, some women experience it during perimenopause, or after menopause. Scientists don’t fully understand what causes menopausal paraesthesia but it may involve changing levels of hormones like oestrogen and their effects on your nervous system and circulation. Paraesthesia can also be caused by a number of other medical conditions. If you have related symptoms or your paraesthesia keeps coming back, you should talk to a doctor. If your doctor thinks your paraesthesia is caused by hormone changes during perimenopause or menopause, they might suggest hormone replacement therapy. Lifestyle changes may also help. Try eating a healthier diet, including a wide range of plants, exercising regularly and, if you smoke, get support with quitting. If you have other menopause symptoms, try the Better Gut probiotic supplement. These award-winning menopause supplements contain beneficial bacteria that have been shown in scientific studies to help with: hot flashes and night sweats mood and symptoms of anxiety and depression brain fog and mental fatigue sleep quality bloating and constipation vaginal health maintaining a healthy weight bone density and osteoporosis risk inflammation and immune health Discover Better Gut and use the discount code WELCOME10 to get 10% off your first order.
Read moreDo menopause hormone changes cause tinnitus, and what can you do?
How changing oestrogen levels may contribute to menopausal tinnitus, the different symptoms you could experience, and treatments that can help.
Read moreEmbracing menopause: Celebrating the second spring of life
As the chill of winter finally begins to fades and the first buds of spring begin to blossom, we find a beautiful metaphor for a significant transition in a woman's life: menopause. In Chinese culture, menopause is poetically termed the 'Second Spring', a period of renewal and rebirth. Whilst it's easy to focus on the challenges this change can bring, let's shift our perspective to embrace the positive transformations during this time, much like the earth rejuvenates and flourishes in spring. The end of winter (menstrual cycles): Just as the cold and dormancy of winter give way to spring, reaching menopause marks the end of menstrual cycles. This transition, though significant, liberates us from the monthly trials of cramps and mood swings, opening a door to newfound freedom and comfort. Blossoming sexuality: Spring is nature's time for growth and renewal, and similarly, post-menopause can be a time of sexual reawakening. Freed from the concerns of pregnancy, intimacy can take on a new spontaneity and joy, blossoming like the flowers of spring. Spring's serenity - calmness and happiness: Imagine the tranquil mornings of spring, the air fresh and calm. Many women find a similar serenity post-menopause. As hormonal fluctuations settle, there's often an increase in overall happiness and a sense of peaceful contentment, much like a spring day. Growing confidence like spring greens: In spring, we see life surge forward with vigour and confidence. Menopause can mirror this natural confidence boost. This time often brings a deeper sense of self, empowerment, and the courage to pursue personal goals and ambitions. Planting new seeds - reflection and change: Spring is a season for planting seeds for future blooms. Menopause offers a parallel opportunity for introspection and life changes. It's a perfect time to evaluate health, lifestyle choices, and to lay down plans for the future – to cultivate the life garden you desire for your years ahead. Much like spring, reaching menopause is just the beginning – a 'Second Spring'. It's a time ripe with potential, growth, beauty and confidence. So as we step into this phase of life, let's do so with optimism, embracing the changes and looking forward to the vibrant possibilities that await us. Let this Second Spring be a celebration of life, a testament to the wisdom and confidence that comes with age, and an opportunity to bloom anew.
Read moreWhy your painful, aching muscles could be menopause, not just age
How hormone changes could be contributing to your increased muscle pain, what symptoms to look out for and what you can do about it.
Read moreIs menopause causing your joint pain, and what can you do?
We look at the link between menopause, hormone levels and joint pain, what it can feel like and the lifestyle changes and supplements that could help.
Read moreWhat’s the connection between menopause and arthritis?
How do changing hormone levels affect your risk of developing osteoarthritis and rheumatoid arthritis, and what can you do about it?
Read moreMenopause hip pain: oestrogen, exercise and gluteal tendinopathy
Exploring the connection between low oestrogen, exercise and hip pain during perimenopause and menopause. Plus, why it’s worse at night and what you can do about it.
Read moreHow do your genetics influence your menopause experience?
Menopause is a significant phase in a woman's life, often accompanied by a variety of symptoms and experiences that can vary greatly from one individual to another. One of the lesser-known factors that can influence this experience is genetics. Understanding the role of genetics in menopause can empower women to make informed decisions about their health and well being during this transition. The power of nutrigenomics in menopause Nutrigenomics is the study of how our genes interact with our diet and lifestyle, and it's particularly relevant to menopause. Our genetic makeup doesn't seal our fate; instead, it provides a blueprint that can be modified by our environment, including the foods we eat and our lifestyle choices. This means that while we can't change our genes, we can influence how they are expressed, effectively turning certain genes "on" or "off" to our advantage. The role of progesterone and oestrogen Two key hormones that are affected during menopause are progesterone and oestrogen. Genetic testing can reveal how efficiently your body processes these hormones. For example, certain genes are responsible for converting progesterone into a calming neurosteroid in the brain, which can affect anxiety levels. Similarly, genes involved in the synthesis and metabolism of oestrogen can influence how your body responds to this hormone during menopause. Personalised nutrition and lifestyle changes By understanding your genetic predispositions, you can tailor your diet and lifestyle to support your hormonal health. For instance, if genetic testing shows that you have a variation that affects how you process progesterone, you might benefit from increasing your intake of vitamin B3, which supports this pathway. Conversely, if you have a genetic variation that makes you less responsive to the calming effects of certain hormones, incorporating herbs like rosemary and lemon balm into your diet might be beneficial. Menopause treatment: one size does not fit all The British Menopause Society acknowledges that menopause treatment should be individualised, taking into account personal and family medical history, symptoms, and preferences. Genetic testing adds another layer to this personalised approach, allowing for more tailored recommendations that go beyond the "one size fits all" model often seen in menopause treatment. Hormone replacement therapy (HRT) and genetics For those considering or currently on HRT, genetic testing can provide insights into how your body might metabolise and respond to supplemental hormones. Understanding your genetic makeup can help you and your healthcare provider make more informed decisions about HRT, potentially reducing the risk of adverse effects and improving the treatment's efficacy. The importance of professional guidance While genetic testing can offer valuable insights, it's crucial to work with a healthcare professional who can help interpret the results and provide recommendations based on your unique genetic profile. A practitioner can guide you through the nuances of nutrigenomics and ensure that you're making the most informed choices for your health. Conclusion Genetics play a significant role in how women experience menopause, but with the advancements in nutrigenomics, it's possible to use this information to your advantage. By understanding your genetic predispositions, you can make targeted changes to your diet and lifestyle that support your hormonal health, potentially leading to a more comfortable menopause experience. Remember, knowledge is power, and in the case of menopause, it can be the key to a better transition. If want to explore your DNA report we have negotiated a great offer with the LifecodeGX team - you can get a full menopause DNA Package RRP: £649.00 for £499 with code TBM at the checkout which includes Lifecode Gx DNA test kit Lifecode Gx Nutrient Core Report Lifecode Gx Hormones Report 30 minute practitioner appointment Understanding your genes enables you to make informed choices to personalise nutrition, lifestyle and other therapeutic approaches to mitigate risks and symptoms - find out more here.
Read more